
Introduction
Timely action has always been central to effective healthcare delivery. The earlier a disease is detected, the greater the range of treatment options and the higher the chances of survival. Unfortunately, across the world, countless patients face diagnostic bottlenecks caused by shortages of specialists, overburdened hospitals, and lengthy diagnostic pathways. What looks like a minor delay on paper can, in practice, be the margin between life and death.
Evidence quantifies the stakes. A meta-analysis in HIV, reported ‘late diagnosis’ in 44% of cases, and a 13% mortality among those diagnosed late. In Systemic Lupus Erythematosus (SLE), median diagnostic delays of nearly 4 years lead to irreversible kidney and cardiovascular complications. In the case of infectious disease, the evidence supports that millions of cases of tuberculosis are left undiagnosed every year due to the massive backlogs in diagnosing that lead to the transmission of the disease. Additionally, a study published in BMJ (British Medical Journal) indicated that every four-week delay along the cancer care pathway increases the risk of deaths by 6 to 13%, depending on the type of treatment.
What these examples illustrate is simple but stark: time lost equals lives lost. This is the context in which artificial intelligence emerges as a transformative force. By rapidly processing medical images, lab data, and patient records, AI helps healthcare systems cut down diagnostic delays while improving accuracy and consistency.
AI as a Game-Changer in Diagnostics
The power of AI lies in its ability to address three persistent bottlenecks: speed, accuracy, and consistency. Human experts, no matter how skilled, are limited by fatigue, workload, and cognitive biases. AI, by contrast, can analyze vast volumes of data in seconds, flagging subtle patterns invisible to the human eye.
Figure 1: Three system-level benefits of AI-based diagnostics
These benefits have been clearly demonstrated in various real-world practices:
- Speed: A recent study showed that AI reduced chest X-ray interpretation time by 42%, from about 34.2 to 19.8 seconds per image, compared with unassisted reading.
- Accuracy: A study from Columbia University demonstrated that the AI model EchoNext could detect structural heart disease (e.g., valve disease, cardiomyopathy) from ECGs with 77% accuracy, outperforming 13 cardiologists who averaged 64% accuracy on the same ECGs.
- Consistency: A formal FDA evaluation of an autonomous diabetic-retinopathy system showed >99% identical outputs on repeat exams across different operators and cameras, indicating highly stable performance across settings.
These results are not limited to just clinics or isolated pilots; major health authorities have cleared AI tools at scale. The U.S. FDA has authorized over 1,000 AI-enabled medical devices, most in diagnostics and particularly imaging. Additionally, in 2021, the World Health Organization endorsed AI-based computer-aided detection (CAD) software for TB X-ray screening in adults, allowing programs to use AI as a substitute for human readers where radiologists are scarce. These examples show that AI is not tied to a single specialty, rather it is reshaping the diagnostic workflow across healthcare.
Beneath these results is a predictable workflow that keeps clinicians in control while the system learns. Data from scans, labs, and records are securely aggregated and standardized; the model produces an initial read; clinicians confirm findings and act; and those outcomes are then fed back to the system to make its performance stronger over time.
Figure 2: AI-Supported Clinical Diagnosis Flow
This closed-loop cycle explains why AI is considered a game-changer, i.e. it doesn’t just accelerate individual diagnoses, it continuously improves itself, while allowing doctors to focus on what matters most – timely, accurate care for patients.
Key Applications of AI in Diagnostics
AI’s role in diagnostics is best understood through the specific domains where it is already transforming the existing practices. Each domain represents a different bottleneck in traditional care, and AI adapts to address those gaps. From medical images to clinical records, these applications demonstrate how technology is being woven into the diagnostic fabric.
Figure 3: Domain areas where AI supports diagnostic decisions

- Medical Imaging: Radiology has been one of the earliest beneficiaries of AI. Algorithms can now flag X-rays, CT scans, MRIs and detect anomalies with a level of precision that often matches or exceeds human interpretation. In practice, this means quicker detection of strokes, tumors, or lung nodules, reducing the chances of delayed treatment. In a large Swedish prospective study, AI-assisted mammography detected 29% more cancers, without increasing false positives and subsequently reduced radiologists’ workload by ~44%. Similarly, for emergency care, Viz.ai’s stroke triage tool has U.S. FDA clearance and demonstrated over 60-minute reductions in door-to-treatment times across multicenter evaluations. Regionally, King Faisal Specialist Hospital & Research Centre in Saudi Arabia has piloted AI solutions for radiology reporting and automated prioritization, integrating them into existing systems.
- Digital pathology and microscopy: AI is now embedded in pathology labs to automate tasks that traditionally require hours of manual slide review. Algorithms assess slide quality, highlight regions of interest, count cells, grade tumors, and quantify immunohistochemistry, with the pathologist validating the final read. Globally, the first FDA De Novo authorization for assistive pathology AI (Paige Prostate) established a regulated workflow for detecting cancer on digitized prostate biopsies, demonstrating accuracy and efficiency gains at scale. In the UAE, Meridian HealthCare deploys digital pathology modules that support whole-slide imaging, automated biomarker quantification, and tissue classification, integrated with hospital systems such as LIS (Laboratory Information System). The result is more consistent counts and grades, shorter turnaround times, and auditable reports for oncology services.
- Tele-diagnostics and Remote Assessment: In many health systems, the first barrier is not technology in hospitals but patients struggling to reach specialists for initial assessment. AI is now filling this gap through conversational chatbots and remote decision-support tools that provide frontline diagnostic guidance. These systems collect symptoms through structured questions, cross-check against clinical knowledge bases, and generate triage recommendations, whether self-care, a GP visit, or urgent referral. Evidence suggests these tools can handle high patient volumes safely. In a 2023 study of virtual health consultations, healthcare providers selected a diagnosis suggested by artificial intelligence in 84.2% of cases. Among these, the AI’s top-ranked diagnosis was correct in 60.9% of the total cases examined. During COVID-19, national health services in the UK and Singapore deployed AI chatbots to screen millions of citizens for symptoms and risk factors, easing pressure on call centers and emergency departments. In Saudi Arabia, Babylon Health in partnership with Saudi Telecom Co. offers an app with AI-based symptom checking and remote consultation features. These tools help with risk assessment and remote diagnosis/triage of common conditions.
- Clinical text and Electronic Health Record Analysis: A major source of delay in diagnosis and treatment is unstructured information such as free-text notes, scattered lab results, and prior patient reports. AI aids by turning this into structured, searchable data. Natural language processing (NLP) can summarize histories, reconcile medications, and extract key clinical features (e.g., symptoms, diagnoses). A 2023 study showed that deep-learning NLP could reliably detect whether ‘goals-of-care’ discussions were documented in free-text clinical notes, achieving over 92% sensitivity, demonstrating how AI can uncover critical information otherwise buried in records. Regionally, Abu Dhabi’s Malaffi health information exchange has introduced an AI-driven Patient Risk Profile that aggregates diagnoses and laboratory data into real-time risk scores for chronic and acute conditions. This approach reduces the time clinicians spend searching across multiple records, illustrating how AI can streamline fragmented data into actionable insight.
- Predictive Diagnostics: Beyond detection, AI models estimate near-term and longitudinal risk, such as infection onset, poor wound healing, or chronic disease progression, by learning from routinely collected variables (demographics, comorbidities, vitals, lab reports, and documented findings). These forecasts support earlier intervention, targeted follow-up, and more efficient resource use.For example, work published in The Lancet Digital Health showed that models trained on standard blood tests predicted type-2 diabetes up to five years before clinical diagnosis, with high accuracy rate. Regionally, Qatar’s Sidra Medicine and Hamad Medical Corporation are advancing AI-enabled genomics programs to anticipate chronic-disease risk at national levels, laying the groundwork for preventive, risk-stratified care.
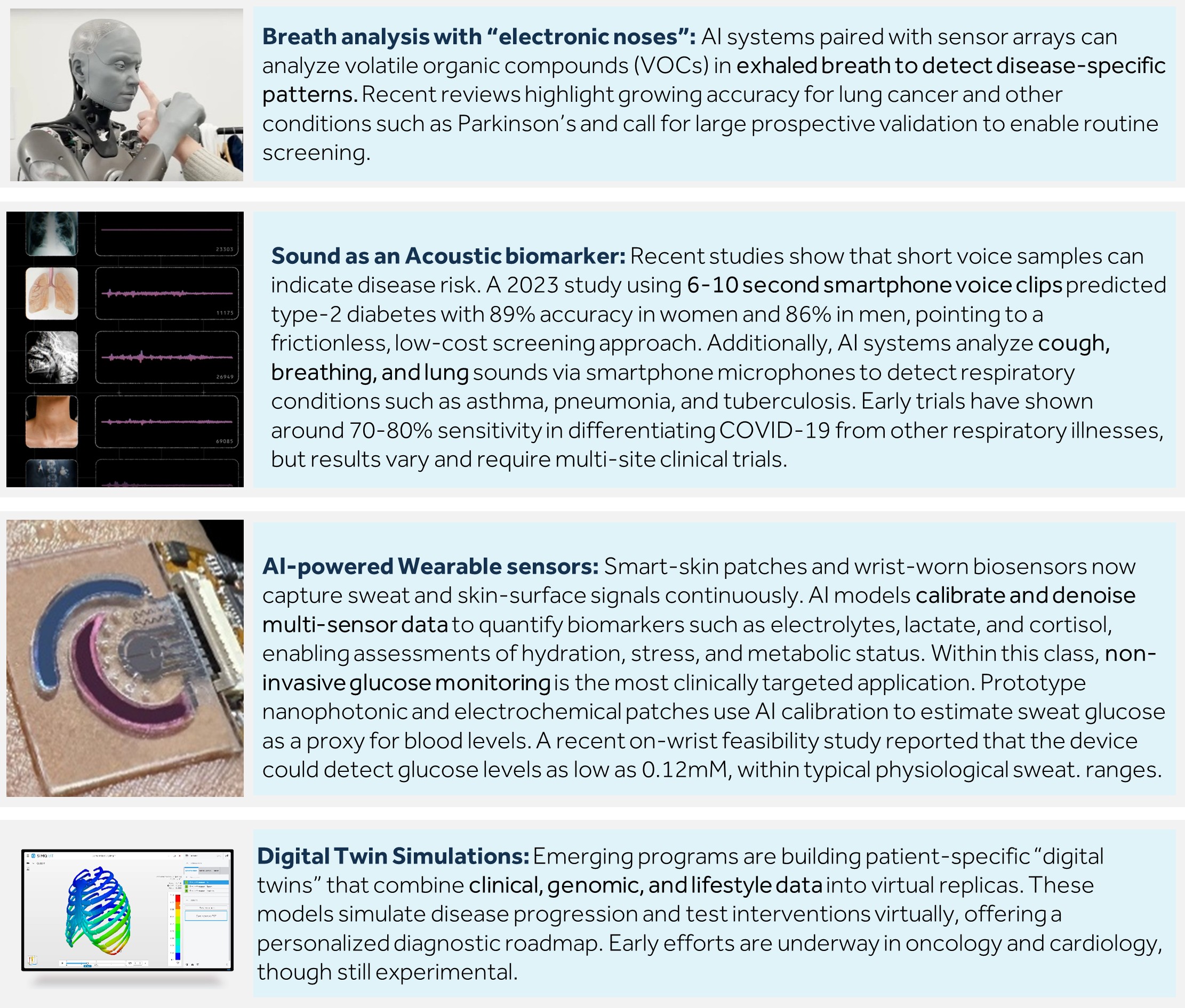
Frontier Innovations in AI Diagnostics
AI is beginning to extract diagnostic signals from routine, everyday inputs, offering screening and continuous monitoring outside traditional tests and clinic visits. Evidence from recent pilots and regulatory evaluations indicates these methods are moving from a mere concept to actual implementation. The section below outlines where they are delivering value today:
Challenges in AI Adoption
The world of AI in healthcare diagnostics holds a lot of promises and potential. However, despite its rapid advancements and impact, AI adoption faces several significant challenges that must be addressed to realize its full potential responsibly and effectively.
- Data quality and bias: AI requires large volumes of high-quality, representative clinical data, yet healthcare data is often fragmented, incomplete, or inaccessible. This not only limits accuracy but can also introduce bias, resulting in unequal diagnostic outcomes across different population groups.
- Model transparency and explainability: The “black box” nature of many AI models makes it difficult to see how they reach their conclusions. Clinicians often cannot trace the reasoning behind an output, which undermines trust and slows adoption in practice. Combined with the need for rigorous clinical validation, this lack of transparency slows trust and uptake in medical practice.
- Regulatory approvals: Navigating the complex landscape of regulatory approvals poses significant challenges. Healthcare diagnostics AI must comply with strict regulatory standards and safety requirements, which often lag behind rapidly evolving AI technologies, resulting in lengthy approval cycles. Additionally, AI relies on processing sensitive patient data, raising issues around consent, data protection, and compliance with regulations like Health Insurance Portability and Accountability Act (HIPAA) and General Data Protection Regulation (GDPR). Managing these concerns requires robust governance frameworks.
- Workflow integration: Integrating AI seamlessly into existing clinical workflows and infrastructure is difficult. Without smooth integration, AI tools risk becoming disruptive or underutilized, while high implementation and maintenance costs further limit uptake, particularly in resource-constrained settings. Clinical validation and building confidence in diagnostic accuracy also require substantial investment.
Addressing these challenges demands coordinated efforts among technologists, healthcare professionals, regulators, and ethicists to develop transparent, equitable, and clinically applicable AI diagnostic solutions that ultimately improve patient outcomes.
The Road Ahead: Toward Predictive, Patient-Centric Care
The next frontier for AI in diagnostics lies not only in faster detection but in shaping a predictive, patient-centric care model. The next wave of diagnostics will detect risk before symptoms by reading signals from wearables, home sensors, and emerging digital biomarkers such as voice or breath. Bedside tools will deliver answers in minutes and reserve invasive testing for confirmation rather than first line. Care plans will adapt to each patient through risk profiles and, when available, digital twins that let teams test options virtually before acting.
To make this real, systems must focus on three enablers. First, data interoperability and security: information must move seamlessly across hospitals, labs, and devices while protecting patient privacy through robust governance and encryption. Second, clinician oversight: AI output must be transparent, explainable, and auditable so doctors remain accountable for final decisions, ensuring technology augments rather than replaces judgment. Third, continuous real-world validation: AI systems must be monitored after deployment to confirm accuracy, fairness, and safety across diverse populations and evolving conditions.
If these pieces come together, the effect will be immense. Decisions will arrive sooner, with fewer low-value procedures. Patients will receive timely, tailored care that keeps them well for longer and the race against time will become a race run ahead of disease.
References:
- National Health Service (2025)
- Medical Lifesciences News (2025)
- Ailoitte (2025)
- GlobalRPH (2025)
- Mayo Clinic (2025)
- Columbia University Irving Medical Center (2025)
- World Health Organization (2025)
- Food and Drug Administration (2025)
- Stop TB (2025)
- Digesitve and Liver Disease (2025)
- TDR WHO (2025)
- PathAI (2025)
- Viz AI (2025)
- Meridian HealthCare AI (2025)
- IQVIA (2025)
- Humanities and Social Science Communications (2025)
- Diagnostic Imaging (2025)
- Nature (2025)
- JMIR Research Protocol (2024)
- Middle East AI News (2024)
- Computer Methods and Programs in Biomedicine Update (2024)
- Clarivate (2024)
- World Economic Forum (2024)
- Dirx Health (2024)
- Hamad Medical Corporation (2023)
- SidraMedicine (2023)
- Biomed Hub (2023)
- The Lancet Oncology (2023)
- Journal of Breast Cancer (2023)
- Mayo Clinic Proceedings: Digital Health (2023)
- Department of Health UAE (2022)
- ACS Omega (2022)
- Memorial Sloan Kettering Cancer Center (2020)
- Klas Research (2020)
- Singapore Economic Development Board (2020)
- Food and Drug Administration (2018)




